UTHealth Houston OMS treats COVID associated avascular necrosis of the maxilla
Published: September 08, 2022 by Kyle Rogers

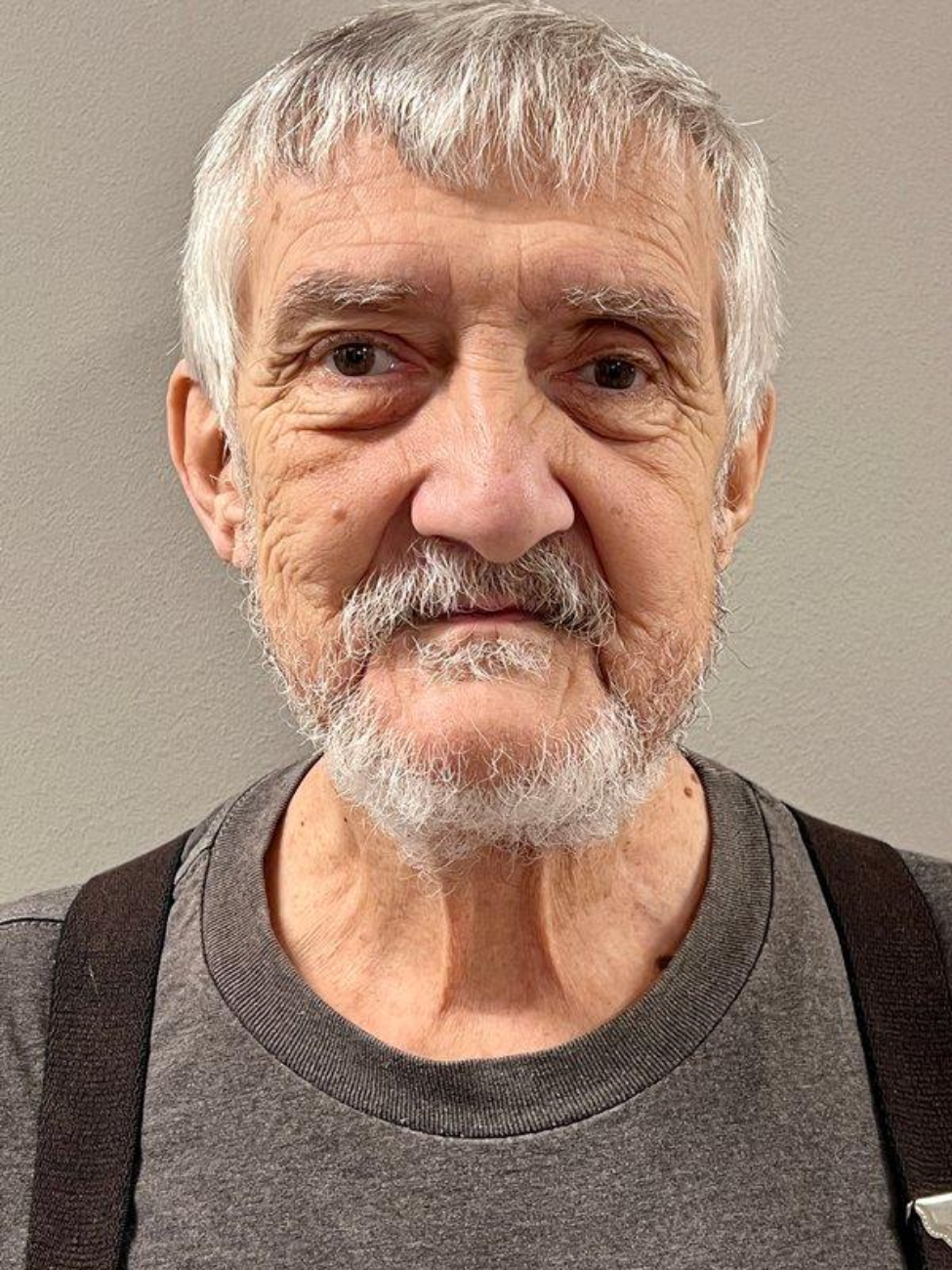
For the better part of two years, 72-year-old William Baker’s health journey has been an uphill climb.
In January 2021, he went to the emergency room with complaints of headaches, blurry vision in his left eye, and loss of taste. However, despite being positive for COVID-19, he was not admitted due to a hospital bed shortage and his comparative state of symptoms.
His case quickly deteriorated due to COVID-related pneumonia and resulted in an extended stay in the intensive care unit. It was during this hospitalization, he also began to develop exposed bone in the left and right maxilla.
Following his discharge, Baker went to a local oral and maxillofacial surgeon in Conroe, Texas, and was subsequently referred to James Melville, DDS, associate professor at UTHealth Houston School of Dentistry and oral surgeon at UTHealth Houston Oral and Maxillofacial Surgeons (UTHealth Houston OMS).
“I’ve had confidence in Dr. Melville since the beginning when I was referred to him,” Baker said. “I was told, ‘He’s the one you need to see.’ There wasn’t any looking around for someone else. I knew he was who could help me.”
Baker presented his case to UTHealth Houston OMS in September 2021.
Clinical examinations revealed extensive complications.
Baker had an edentulous maxillary ridge with exposed, infarcted bone on the labio-buccal surface extending from his left posterior maxilla anteriorly to the left canine region and from the keratinized gingiva mid-height of the alveolus to the depth of the vestibule. He also had an isolated, 8-by-8-millimeter segment of the infarcted bone present on the labial surface of the right maxilla in the premolar region, which was suppurative.
A maxillofacial CT revealed osteolytic changes of the hard palate, superior alveolar ridge, left maxilla, zygoma, zygomatic arch, left ethmoid air cells (lamina papyracea), pterygoid plates, and pterygoid palatine fissure.
Additionally, a neck CTA demonstrated an abrupt cutoff of a small branch of the left internal maxillary artery located adjacent to the medial aspect of the left mandible, representing occlusion. The left pterygoid plexus was nonfilling, indicating further occlusion of these branches.
For his treatment, Melville and UTHealth Houston OMS performed two surgeries.
The first surgery was in January 2022 for debridement of the maxilla. Melville was the attending surgeon. He was assisted by OMS residents Steven Balandran, DDS, MD; Duc Lam, DDS, MD; Victoria Mañón, DDS, MD; Maxime Fournier, DDS; and Jamie Choi, DDS, MD.
“Due to the extensive nature of the avascular necrosis and infection, we delayed a definitive free flap reconstruction,” Melville said. “We hoped that a buccal fat pad and adjacent mucosal closure would hold up, but he eventually developed a large sinus opening.”
While Baker was in recovery, UTHealth Houston OMS published work on the case, titled “COVID-Associated Avascular Necrosis of the Maxilla-A Rare, New Side Effect of COVID-19,” in the July issue of the Journal of Oral and Maxillofacial Surgery.
Upon recovery, Melville and UTHealth Houston OMS performed a radial forearm free flap reconstruction surgery to close Baker’s sinus from his mouth in July 2022.
Two teams performed the surgery. Melville once again served as the attending surgeon, leading a team on the free flap reconstruction, while Jonathan Shum, DDS, MD, led another team in locating neck vessels to connect to as well as preparing the remaining maxilla to receive the free flap. Maxillofacial Oncology and Reconstructive Fellows Brain Rethman, DMD; and Salah Al Din Al-Azri, BDS, MD; and OMS residents Omar Ahmed, DDS; Steven Balandran, DDS, MD; Christopher Midtling, DDS, MD; and Rishabh Rattan, DDS, aided in the procedure.
“The flap will eventually heal and shrink down to look natural, and the arm will heal on its own, too,” Melville said. “At his September post-operation appointment, Mr. Baker has healed well and will be back to his normal life—eating, drinking, and speaking—before the COVID maxilla.”
Baker praised Melville and UTHealth Houston OMS for taking his case and getting him on the road to recovery.
“They’re terrific,” Baker said. “Throughout this experience, I’ve known I had the best doctors available to take care of me.”
Baker also notes how the care he has received has given him a positive outlook for the future for the first time since his COVID-positive diagnosis.
“It’s been a very rough road,” Baker said. “After all this—getting COVID and the complications, aches, and pains—I feel like it’s ok to live, again. After the healing, I look forward to getting my energy back, and then it will be my wife telling me to ‘slow down.’”
Surgical assistants on Baker’s case were Rosa Benavidez and Rosie Sanchez, and patient care coordinators were Dena McDaniel and Shymira Crowly-Fredrick.

