Labs
UTHealth Houston School of Dentistry houses a research department that performs innovative and cutting-edge basic, clinical, and educational research.
Research at UTHealth Houston School of Dentistry drives innovation in the dental profession through cutting-edge basic, translational, and clinical studies aimed at improving patient care and clinical practice.
The research mission of UTHealth Houston School of Dentistry is to conduct basic, clinical, and translational research on the orofacial complex and related aspects of systemic health in order to improve the well-being of our patients and the community.
To be leaders in understanding the etiology and pathogenesis of common and complex oral conditions that impact the quality of life of our patients.
UTHealth Houston School of Dentistry houses a research department that performs innovative and cutting-edge basic, clinical, and educational research.
The School of Dentistry houses the Center for Craniofacial Research, the Houston Center for Biomaterials and Biomimetics, and the Texas Center for Oral Healthcare Quality and Safety.
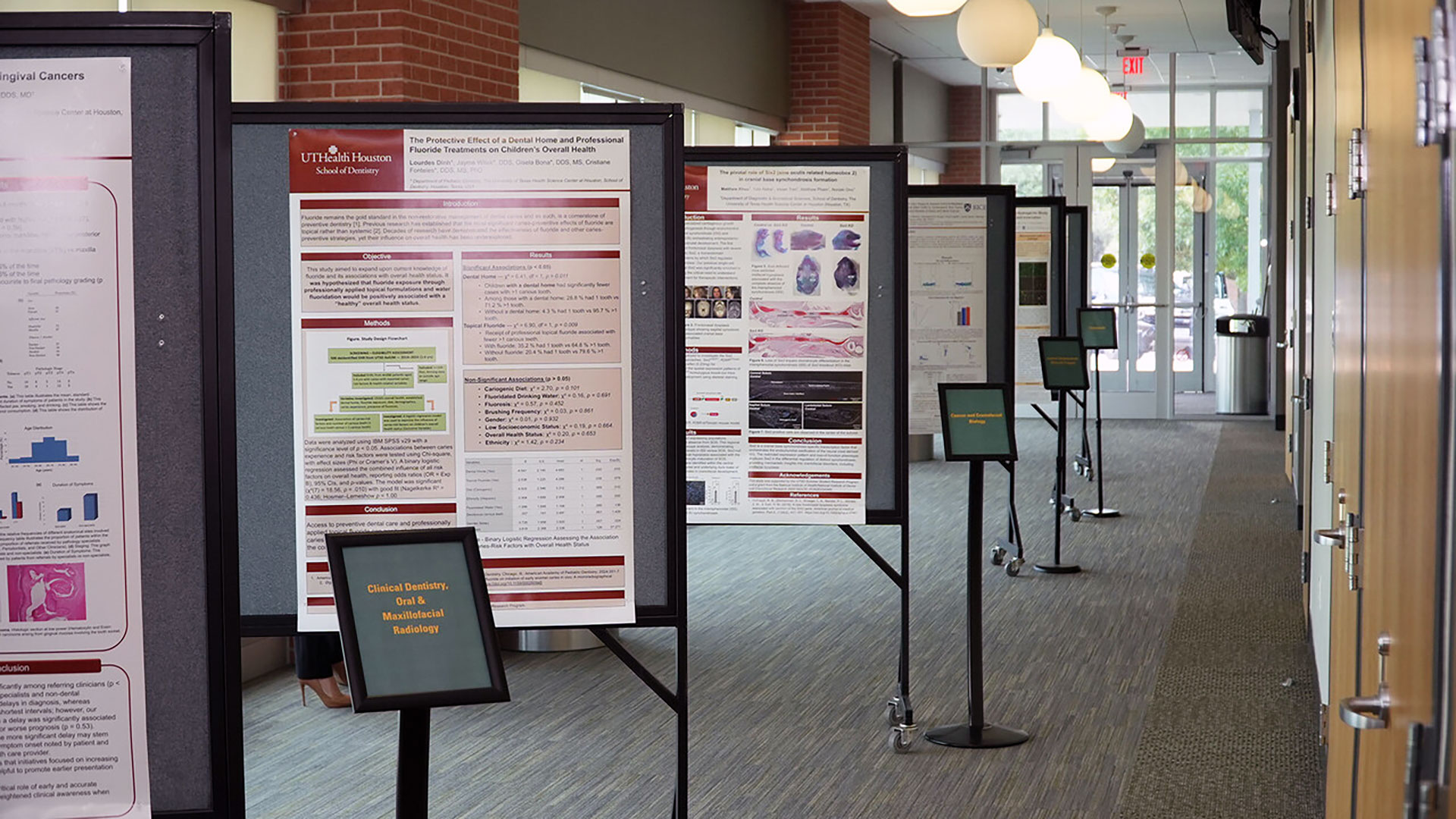
The Student Research Group promotes, supports, and nurtures the interests of dental student researchers during their time at the school.
The Houston Section has been established to promote the mission and objectives of the American Association for Dental, Oral, and Craniofacial Research (AADOCR) on a local level, in abidance with the rules and regulations of that organization. The foremost purpose of this Section is to encourage research collaboration, support, and represent the oral health research community of Houston with the goal of contributing to the advancement of oral health worldwide.


For Grants/Contract related needs:
[email protected]
For IRB/iRIS related needs:
[email protected]